BARCELONA, Spain - New data have shown that first-line treatment with a combination of two immunotherapy drugs improves overall survival in a subset of patients with advanced non-small cell lung cancer (NSCLC) compared to chemotherapy (1).
The data from the CheckMate-227 trial, reported at the ESMO Congress 2019, suggest that the combination of nivolumab plus low-dose ipilimumab could offer a chemotherapy-free option for first-line treatment of patients with advanced NSCLC. Nivolumab, a PD-1 antibody, and ipilimumab, an anti-cytotoxic T-lymphocyte antigen 4 (CTLA-4) antibody, are immune checkpoint inhibitors with distinct but complementary mechanisms of action.
“In my opinion these data are practice changing. CheckMate-227 is the first trial showing that the combination of nivolumab and ipilimumab prolongs survival as compared to chemotherapy in treatment-naïve patients with metastatic NSCLC,” said study first author Prof. Solange Peters, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland. “We already have several front-line treatment options for these patients, including chemotherapy combined with an anti-PD1 agent or an anti-PDL1 agent alone. And now we have a chemotherapy-sparing option of nivolumab plus ipilimumab.”
Peters added, “The important step now is to develop an algorithm to select the best front-line treatment for each patient. We need to wait for a little more time to see which treatment really gives rise to improved long-term survival. The five-year survival from trials with these treatments will teach us if any of the options are better than others. The second critical point will be to compare toxicities. We can then have an informed discussion with our patients.” She noted that CheckMate-227 showed that safety profiles of both strategies are different, in terms of specific toxicity events encountered, their timing, grade and prevalence, with diarrhoea, rash and fatigue being the most common adverse events with nivolumab/ipilimumab and fatigue, gastrointestinal and haematological toxicities with chemotherapy. “We used a low dose of ipilimumab (1mg every 6 weeks) to make it tolerable. Doing this led to a low rate of discontinuation and treatment-related toxicities or deaths. So it’s a highly manageable treatment.”
Considering the limitations of the trial, Peters explained that it started before chemotherapy/immunotherapy or immunotherapy alone was approved for the front-line treatment of NSCLC, so the two-drug immunotherapy combination was not compared with current standards of care. “Unfortunately, we did not include a treatment arm with the combination of chemotherapy plus nivolumab in the PD-L1 positive cohort, but only in the negative one,” she said. However, an exploratory analysis suggested that nivolumab/ipilimumab was more effective than nivolumab alone in the PD-L1 positive group, which was more effective than chemotherapy. Additionally nivolumab/ipilimumab demonstrated a higher activity than nivolumab combined with chemotherapy in PD-L1 negative patients.
Another limitation was that the trial was designed to formally assess overall survival in patients who were positive for PD-L1. “But we looked in an exploratory fashion at the subgroup of patients who were negative for PD-L1. Similarly to patients who were positive for PD-L1 the benefit with nivolumab/ipilimumab was seen across variable levels of PD-L1 expression, including negative ones,” said Peters.
Commenting on the relevance of the new data, Dr Marina Chiara Garassino, Istituto Nazionale dei Tumori, Milan, Italy, said, “These data show we have a new treatment option for the first-line treatment of metastatic NSCLC, to add to the current treatment options of chemotherapy plus immunotherapy regardless of PD-L1 level or immunotherapy as single agent for patients with PD-L1 scores of at least 50%.” But she cautioned, “We don’t yet know if the findings are practice changing. We need to understand which treatment is best for each patient: chemotherapy plus immunotherapy, immunotherapy alone or immunotherapy plus immunotherapy.” She considered more information is needed on biomarkers to individualise therapy.
Garassino agreed on the limitation of CheckMate-227 to have started before the introduction of current standards of care. “The comparison was chemotherapy alone, but this is no longer the standard for patients with metastatic NSCLC,” she said.
Study results
The global phase 3 CheckMate-227 study included patients with stage IV or recurrent NSCLC who had received no previous treatment. Part 1 of this multipart study was designed to evaluate different nivolumab-based regimens versus chemotherapy in two different PD-L1 subgroups.
In part 1 of the trial, patients with PD-L1 expression of at least 1% (n=1,189 patients) were randomized to three treatment options: nivolumab plus low-dose ipilimumab, nivolumab or histology-based chemotherapy. Patients with PD-L1<1% (n=550) were randomised to nivolumab plus low-dose ipilimumab, nivolumab plus chemotherapy or chemotherapy.
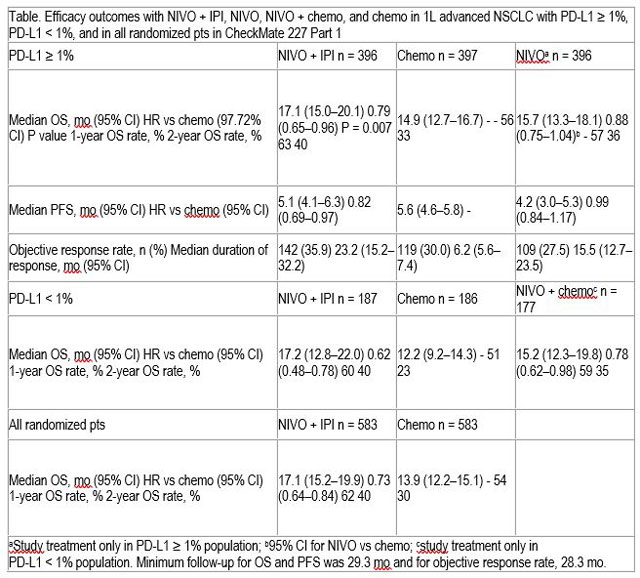
Overall survival was significantly longer with nivolumab plus ipilimumab compared to chemotherapy. Patients with PD-L1>1% treated with nivolumab plus ipilimumab had a median overall survival of 17.1 months (95% confidence interval [CI] 15.0-20.1 months) compared to 14.9 months (95% CI 12.7-16.7 months) in the chemotherapy group (hazard ratio [HR] 0.79, 97.72% CI 0.65-0.96, p=0.007).
Progression-free survival, objective response rates and duration of response were all greater with nivolumab plus ipilimumab compared to chemotherapy.
Overall survival also showed benefit with nivolumab plus ipilimumab vs chemotherapy in patients with PD-L1<1% and in all randomised patients (those with PD-L1<1% and >1%)
The rate of grade 3-4 treatment-related adverse events across all patients was 33% in those treated with nivolumab plus low-dose ipilimumab, 19% with nivolumab and 36% with chemotherapy.
Official Congress Hashtag: #ESMO19
Social Media information:
Reference
- Abstract LBA7128 ‘Nivolumab (nivo) + low-dose ipilimumab (ipi) vs platinum-doublet chemotherapy (chemo) as first-line (1L) treatment (tx) for advanced non-small cell lung cancer (NSCLC): CheckMate-227 part 1 final analysis’ will be presented by Solange Peters during the Presidential Symposium I on Saturday, 28 September, 16:30 to 18:20 (CEST) in Barcelona Auditorium (Hall 2). Annals of Oncology, Volume 30, Supplement 5, October 2019
LBA4_PR - Nivolumab (NIVO) + low-dose ipilimumab (IPI) vs platinum-doublet chemotherapy (chemo) as first-line (1L) treatment (tx) for advanced non-small cell lung cancer (NSCLC): CheckMate 227 Part 1 final analysis
S. Peters1, S.S. Ramalingam2, L. Paz-Ares3, R. Bernabe Caro4, B. Zurawski5, S.-W. Kim6, A. Alexandru7, L. Lupinacci8, E. de la Mora Jimenez9, H. Sakai10, I. Albert11, A. Vergnenegre12, M. Reck13, H. Borghaei14, J.R. Brahmer15, K.J. O'Byrne16, W.J. Geese17, P. Bhagavatheeswaran17, F.E. Nathan18, M.D. Hellmann19
1Multidisciplinary Oncology Center, Centre Hospitalier Universitaire Vaudois - CHUV, Lausanne, Switzerland, 2Hematology And Medical Oncology, Emory University, Winship Cancer Institute, Atlanta, United States of America, 3Medical Oncology, University Hospital 12 De Octubre, Madrid, Spain, 4Medical Oncology Department, Hospital Universitario Virgen Del Rocio, Seville, Spain, 5Chemotherapy Department, Ambulatorium Chemioterapii, Bydgoszcz, Poland, 6Department Of Oncology, Asan Medical Center, Seoul, Korea, Republic of, 7Medical Oncology Department, Institute Of Oncology "Prof. Dr. Alexandru Trestioreanu" Bucha, Bucharest, Romania, 8Clinical Oncology, Hospital Italiano, Buenos Aires, Argentina, 9Medical Oncology Department, Instituto Jalisciense De Cancerología, Jalisco, Mexico, 10Thoracic Oncology Department, Saitama Cancer Center, Saitama, Japan, 11Pulmonary Department, Matrai Gyogyintezet, Matrahaza, Hungary, 12Uotc Department- Unité Oncologie Thoracique Et Cutanée, CHU Limoges - Hopital Dupuytren, Limoges, France, 13Thoracic Oncology, Lung Clinic Grosshansdorf, Airway Research Center North, German Center of Lung Research, Grosshansdorf, Germany, 14Hematology And Oncology, Fox Chase Cancer Center, Philadelphia, United States of America, 15Oncology Department, Sidney Kimmel Comprehensive Cancer Center At Johns Hopkins, Baltimore, United States of America, 16Cancer Services, Princess Alexandra Hospital, Woolloongabba, Australia, 17Global Biometric Sciences, Bristol-Myers Squibb, Princeton, United States of America, 18Oncology Clinical Development, Bristol-Myers Squibb, Princeton, United States of America, 19Medical Oncology, Memorial Sloan Kettering, New York, United States of America
Background: Part 1 of CheckMate 227 (NCT02477826), a phase 3 study in 1L NSCLC, has dual primary endpoints. The primary endpoint of progression-free survival (PFS) with NIVO + IPI vs chemo in patients (pts) with tumor mutational burden ≥ 10 mut/Mb was met, as reported previously. Here we present the primary endpoint of overall survival (OS) for NIVO + IPI vs chemo in pts with tumor PD-L1 expression ≥ 1%.
Methods: Pts were chemo-naive, with stage IV or recurrent NSCLC without EGFR or known ALK alterations, ECOG PS 0–1. Pts with PD-L1 ≥1% (n = 1189) were randomized 1:1:1 to NIVO 3 mg/kg Q2W + IPI 1 mg/kg Q6W, NIVO 240 mg Q2W, or histology-based chemo; pts with PD-L1 < 1% (n = 550) were randomized 1:1:1 to NIVO 3 mg/kg Q2W + IPI 1 mg/kg Q6W, NIVO 360 mg Q3W + chemo, or chemo. Pts were stratified by histology in both populations. Pts were treated until disease progression, unacceptable toxicity, or for 2 y of immunotherapy.
Results: Baseline characteristics were balanced across tx arms. Minimum follow-up for the primary endpoint was 29.3 mo. For pts with PD-L1 ≥ 1%, OS was significantly longer with NIVO + IPI vs chemo (HR 0.79, 97.72% CI: 0.65–0.96; P = 0.007); PFS, objective response rates, and duration of response favored NIVO + IPI vs chemo. OS benefit was also observed in pts with PD-L1 < 1% and all randomized pts (Table). Prespecified analyses showed enhanced efficacy with NIVO + IPI relative to NIVO in PD-L1 ≥ 1% and relative to NIVO + chemo in PD-L1 < 1%. Grade 3–4 tx-related adverse event rates in all randomized pts were 33% with NIVO + low-dose IPI, 19% with NIVO, and 36% with chemo.
Conclusions: CheckMate 227 met its primary endpoint of significantly improved OS with NIVO + IPI vs chemo in 1L advanced NSCLC with PD-L1 ≥ 1%. OS was also improved with NIVO + IPI in PD-L1 < 1% and in all randomized pts. Safety profile was consistent with previous reports in NSCLC. NIVO + IPI represents a new chemo-free tx option for pts in 1L advanced NSCLC.
Clinical trial identification: NCT02477826 Release date: June 23, 2015
Editorial acknowledgement: Writing and editorial assistance was provided by Namiko Abe, PhD, of Caudex, funded by Bristol-Myers Squibb.
Legal entity responsible for the study: Bristol-Myers Squibb
Funding: Bristol-Myers Squibb
Disclosure: S. Peters: Advisory / Consultancy, Research grant / Funding (institution): Abbvie, Amgen, AstraZeneca, Bayer, Biocartis, Bioinvent, Blueprint Medicines, Boehringer-Ingelheim, Bristol-Myers Squibb, Clovis, Daiichi Sankyo, Debiopharm, Eli Lilly, F. Hoffmann-La Roche, Foundation Medicine, Illumina, Janssen, Merck Sharp and Dohme, M.
S.S. Ramalingam: Research grant / Funding (institution): Bristol-Myers Squibb; Honoraria (self), Advisory / Consultancy, Research grant / Funding (institution), Personal fees, advisory board: Amgen; Honoraria (self), Advisory / Consultancy, Personal fees, advisory board: AbbVie; Honoraria (self), Advisory / Consultancy, Personal fees, advisory board: Lilly; Honoraria (self), Advisory / Consultancy, Personal fees, advisory board: Genentech; Honoraria (self), Advisory / Consultancy, Research grant / Funding (institution), Personal fees, advisory board: Takeda; Honoraria (self), Personal fees: Loxo; Research grant / Funding (institution): Advaxis; Honoraria (self), Research grant / Funding (institution), Personal fees: Tesaro; Honoraria (self), Research grant / Funding (institution), Personal fees: Merck; Honoraria (self), Research grant / Funding (self), Personal fees: Astra Zeneca.
L. Paz-Ares: Advisory / Consultancy, Advisory board: Genómica; Honoraria (self), Personal fees: Lilly, MSD, Roche, Pharmamar, Merck, AstraZeneca, Novartis, Boehringer Ingelheim, Celgene, Servier, Sysmex, Amgen, Incyte, Pfizer, Ipsen, Adacap, Sanofi, Bayer, Blueprint, Bristol-Myers Squibb; Advisory / Consultancy, Scientific advice/speaker: Lilly, MSD, Roche, Pharmamar, Merck, AstraZeneca, Novartis, Boehringer Ingelheim, Celgene, Servier, Sysmex, Amgen, Incyte, Pfizer, Ipsen, Adacap, Sanofi, Bayer, Blueprint, Bristol-Myers Squibb; Officer / Board of Directors, Co-founder and board member: Altum Sequencing; Research grant / Funding (institution), Grant: MSD, AstraZeneca, Pfizer, Bristol-Myers Squibb.
H. Sakai: Research grant / Funding (institution), Grant: Ono Pharmaceutical Company, Bristol-Myers Squibb Company, AstraZeneca, Chugai Pharmaceutical Company, Merck & Co, Merck KGaA; Honoraria (self), Personal fees: Ono Pharmaceutical Company, Bristol-Myers Squibb Company, AstraZeneca, Chugai Pharmaceutical Company, Merck & Co, Merck KGaA.
A. Vergnenegre: Honoraria (self), Advisory / Consultancy, Personal fees, travels for medical conferences and fees for consulting: Bristol-Myers Squibb, MSD, AstraZeneca.
M. Reck: Honoraria (self), Advisory / Consultancy, Honoraria for lectures and consultancy: AbbVie, Amgen, AstraZeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Celgene, Lilly, Merck, MSD, Novartis, Pfizer, Roche.
H. Borghaei: Research grant / Funding (institution): Millennium, Merck/Celgene, Bristol-Myers Squibb/Lilly; Advisory / Consultancy: BMS, Lilly, Genentech, Celgene, Pfizer, Merck, EMD-Serono, Boehringer Ingelheim, Astra Zeneca, Novartis, Genmab, Regeneron, BioNTech, Cantargia AB, Amgen, Abbvie, Axiom, PharmaMar, Takeda, Huya Bio, Diiachi; Advisory / Consultancy, Data Safety and Monitoring Board: University of Pennsylvania, CAR T Program; Takeda; Full / Part-time employment: Fox Chase Cancer Center.
J.R. Brahmer: Advisory / Consultancy, Research grant / Funding (institution), Grant, advisory board: Bristol-Myers Squibb; Advisory / Consultancy, Advisory board: AstraZeneca, Genentech, Merck.
K.J. O'Byrne: Advisory / Consultancy, Speaker Bureau / Expert testimony, Advisory board and speaker bureau fees and travel grants to national and international meetings: Bristol-Myers Squibb, Pfizer, AstraZeneca, MSD, Roche-Genentech, Boehringer-Ingelheim; Advisory / Consultancy, Advisory board: Novartis, Teva, Natera; Advisory / Consultancy, Speaker Bureau / Expert testimony, Advisory board and speaker bureau fees: Janssen-Cilag; Speaker Bureau / Expert testimony, Speaker bureau: Mundipharma; Shareholder / Stockholder / Stock options, Shareholder: Carp Pharmaceuticals, Carpe Vitae Pharmaceuticals; Licensing / Royalties, Various patents issues with licensee as listed: Queensland University of Technology and Trinity College Dublin.
W.J. Geese: Shareholder / Stockholder / Stock options, Full / Part-time employment: Bristol-Myers Squibb.
P. Bhagavatheeswaran: Shareholder / Stockholder / Stock options, Full / Part-time employment: Bristol-Myers Squibb.
F.E. Nathan: Full / Part-time employment: Bristol-Myers Squibb.
M.D. Hellmann: Advisory / Consultancy, Fees for consulting: Genentech, Merck, Novartis, Janssen, Mirati, Syndax, Nektar, Blueprint Medicines; Advisory / Consultancy, Research grant / Funding (institution), Research grant to institution, fees for consulting and travel (grant, personal fees, non-financial support): Bristol-Myers Squibb; Advisory / Consultancy, Fees for consulting and travel: AstraZeneca; Advisory / Consultancy, Fees for consulting and equity: Shattuck Labs, Immunai; Licensing / Royalties, Patent filed by Memorial Sloan Kettering related to the use of tumor mutation burden to predict response to immunotherapy: PGDx.
This press release contains information provided by the author of the highlighted abstract and reflects the content of this abstract. It does not necessarily reflect the views or opinions of ESMO who cannot be held responsible for the accuracy of the data. Commentators quoted in the press release are required to comply with the ESMO Declaration of Interests policy and the ESMO Code of Conduct.